This article appears in the November 2005 edition of the Catholic Medical Quarterly
Euthanasia -What it is and What it is Not
Ilora Finlay of Llandaff
Reproduced by kind permission of Dolentium Hominum
Voluntary Euthanasia is the deliberate administration of a drug with the purpose (intention) of bringing about the death of a patient at his/her competent and persistent request. When the patient takes the prescribed lethal medication without help, the term ‘physician assisted suicide’ is used. However, this is inextricably linked to euthanasia because, if the patient for some reason cannot take the drug unaided, then they will request assistance. Additionally if the attempt to kill oneself through swallowing a lethal dose of drug, usually barbiturate, fails, then the patient is killed with a lethal injection.
Other terms, such as non voluntary, involuntary and passive euthanasia, are used to describe the process of end of life decisions making, but the term voluntary euthanasia should be strictly reserved for the deliberate ending of a life at a specified and predicted time according to the definition above. It is misleading to attach the word euthanasia to these other situations. Involuntary euthanasia is the killing of a patient without their request - it is murder or manslaughter depending on the circumstances; it was practised by the Nazis in the early 1930s when those with mental illness and disability were `relieved of a life not worth living'. Non-voluntary euthanasia is the ending of a life at the explicit request of another - usually a close relative - but without the explicit request of the patient because they lack competence; again this is manslaughter.
Passive euthanasia is the most misleading of all the terms as it implies that the withdrawing or withholding of treatment always has the intention to cause death. However, this is a very difficult scenario when a patient is gravely ill; the disease process is taking them inexorably towards death. The stopping of medication may not bring about their death - indeed it may surprisingly result in clinical improvement. It is worth remembering that, during the doctors' strike in Israel, the death rate went down! Every clinician will recall patients who were thought to be imminently dying and surprisingly rallied the following day, just as there are many who seem to have a life expectancy of some weeks and suddenly die. The decision to withhold medication is taken on the balance of harms - if the considered intervention is predicted to be more burdensome or risky than its predicted benefits, then it should not be given. Such predicted balancing of benefits against risks and burdens requires consideration of the principle of justice, since with limited resources the use of an intervention on one patient may deprive another who has a greater chance of benefiting. Such is the decision that clinicians face when there are limited numbers of ventilators or other high technology or expensive possibilities, and brings the debate over end of life decision making into the arena of rationing. Although the outcome may be the same as in euthanasia - the patient's death - the fundamental intention is different and the decision making process very different. However, even ceasing ventilation can sometimes result in the patient surprisingly starting to breathe spontaneously.
Some philosophers and ethicists disagree with this analysis, but theory and practice are differentiated by the subtleties of the clinical decision-making process, not only the outcome. It can be useful to think about a patient as travelling down a path towards death. If treatment is withheld or withdrawn at point A the patient is predicted to die but the time is uncertain - it may occur at point B, C or D in the diagram below. So, the true prognosis cannot be accurately predicted, the disease is progressing and intervention may (or may not) alter the course towards death.
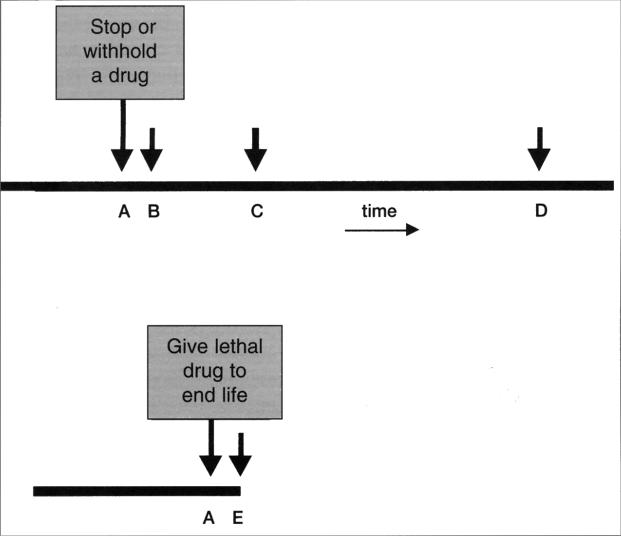
However, if euthanasia is practised, the patient will certainly be dead within the time from giving the drug at time A and the predictable end-point of death at E. The sole purpose of the euthanasia is to kill the patient at their competent and persistent request; there is no room for life to continue.
So, euthanasia is not the withdrawing or withholding of treatment that has no purpose and affords no benefit to the patient as a person. The patient may live for a long or short time after the decision, until natural death occurs, due to the underlying disease process. But, euthanasia is the deliberate administration of a lethal dose to cause certain death at a set time.
Different phrases have been used by advocates of euthanasia, as euphemisms for the process. ‘Death with dignity’ implies that the only way a person can die with dignity is to have euthanasia; yet the palliative care movement has been striving to ensure that everyone has a dignified natural death. The term ‘right to die’ has been used to describe the demand for a change in the law to permit euthanasia; however, since everyone will die inevitably, this is a universal ‘right’ the advocates of euthanasia are asking for the right to be killed.
The term ‘assistance in dying’ has been used to describe the process - indeed it is in the title of the Bill - The Assisted Dying of the Terminally Ill Bill - currently before the UK Parliament. But, as the Royal College of Nursing have pointed out in their oral evidence to the House of Lords Select Committee that has been set up to examine this Bill, those giving palliative care are like midwives. A midwife is present at birth to assist the natural process. Similarly at death the palliative care team are there to ease the natural process, not hasten it or defer it.
Prognosis prediction is notoriously difficult. All doctors have had patients under the care who look as if they are dying soon, but make a dramatic recovery, sometimes to live for months or years. Others who look as if they will live for months are dead in days or weeks. Any prognosis prediction based on probabilities is just that - it is a best guess from the data available; but there is no accurate way of predicting the prognosis of a patient, even those with advanced cancer. In those with neurological disease or cardiac disease, it is even harder to hazard a guess at life expectancy. Work by Paul Glare in Australia has demonstrated just how inaccurate prognosis prediction can be, even in advanced cancer.
When a euthanasia request is made it is crucial to be certain that the patient is not under duress and, therefore, that they are competent to make such a request. For consent to any intervention to be valid, it must be voluntary. The patient must be fully informed of the process and possible outcomes, including complications, and must be able to understand the implications for him/herself and for others. There must be no distortion of thinking through depression, drugs etc. and the patient must be able to communicate the request.
Thus the very people that may be considered to be the most likely to ‘warrant’ euthanasia in society's eyes are the very people who are not eligible, as they cannot make a valid, competent request. How often does one hear it said ‘you would not let a dog be like that’ of a patient who is demented or profoundly psychiatrically disturbed. But people are not dogs; and those with impaired competence are the most vulnerable in our society, in need to be protected from harm inflicted by self or others.
The way that a clinician, be it doctor or nurse, communicates with a patient gives a very powerful message about the future of that patient. The patient is extremely dependent on the clinical team: they are the source of most information about the disease, the ones who can provide adequate symptom relief if they have the knowledge and can be the access to all sorts of treatment. So the unequal position of power should not be underestimated. Unfortunately since many clinicians have not had adequate communication skills training, they are not as skilled as they should be at entering into two way dialogue with patients. Many spend far too much time in consolation talking to the patient rather than listening to the patient's concerns; as a rule of thumb it is worth remembering that whoever provides a support service should listen for about 80% of the time and speak for only about 20% of the time on average. In a consultation, the commonest complaint of patients is that they were not listened to. The culture of an institution also alters communication. In those teams where there is open communication, then communication with patients seems to be better. Those health care professionals who are able to talk about their own death are more comfortable talking with patients about death and dying, thus are more able to allay fears and address concerns.
Patients who desire death often cite fear of being a burden to others as their main reason. This concern was exemplified by a group of patients in a study discussing issues of spirituality in advanced disease. They did not want to be a burden to their family. As one woman said: ‘They have to live with it after you have gone, and that's the hardest, what you have burdened them with is what they will remember’.
This concept of the family having to live with the memories they have of a person as a patient, rather than when they were fit and healthy, is also very strong and motivates many to struggle on, not disclosing that they need additional help and support. Another woman described: "My boy said: ‘Why are you always laughing, why are you always smiling?’ I said: ‘Because I don't want you to remember me as miserable. I want you to remember me laughing and smiling."
The burden of being ill weighs heavily on some patients, creating 'a sense of isolation: `You find you can't talk to your family about your illness because they can't handle it. It becomes a burden that presses you down sometimes, so that you just want to scream and shout and tell them how you really feel. But you can't because they just can't cope with it. They are just about hanging on as it is'.
Dignity has been defined, by the founder of the modern hospice movement, Cicely Saunders, as having a sense of personal worth. A perception of loss of dignity has been associated with desire for death as demonstrated by the work of Harvey Chochinov. Those patients reporting moderate or severe loss of dignity were more likely to desire death, had higher sense of being a burden and higher levels of anxiety. Their sense of dignity was highly dependent on the time of care given. Thus, again, the power of the professionals to influence how the patient views their life cannot be underestimated. Indeed, Chochinov has suggested that: ‘Care, that confers honour, recognised the deservedness of respect and esteem of every individual - despite their dependency, infirmity and fragility - could lie at the heart of care that conserves dignity’.
Amongst those who desire death to be brought forward, a few key characteristics emerge: these patients experience a sense of loss of connectedness to the world around them - they have experienced social death, where the roles they once had are taken by others and they feel society behaves as if they were already dead. They often fear the future, viewing it as holding more horrors than the present. They are profoundly influenced by bad past experiences, particularly if they have seen a loved one die badly, even many years ago. Pain and other symptoms do not seem to be a major issue, although profound weakness and fatigue are demoralising. Such patients often have great fear of being a burden; they may view the process of needing care as humiliating and maybe experiencing poor care.
Interviews with patients who request physician-assisted suicide in Oregon reveal the same picture as in Europe Linda Ganzini reports such patients as being people who value control, dread dependence, and assess their current quality of life as poor. They have often been high achievers in life and find palliative care difficult, as they deplore needing care. Additionally: ‘Many tell of childhood experiences with unempathic and over-controlling adult figures where they learned that receiving care from others is humiliating.’
These patients report higher levels of physical symptoms and psychological suffering than those not requesting death. The fear of being a burden and needing care is coupled with a sense of being demoralised by the process of being ill, by depression or both. They report less confidence in symptom control, fewer social supports and overall less satisfaction with life experiences. Those over 65 years of age are more likely to feel unappreciated than those who do not express a desire for death.
Kissane and other researchers have found that those desiring death are often depressed, demoralized or both. They seem also to have doctors who are demoralized by the process of giving care and are somewhat worn down by it, suggesting that the doctor's mood may be a powerful influence on the patient's perception.
Those who advocate euthanasia are often motivated by their own experiences in the past of seeing someone they love die in pain or in distress. Sometimes the pain and suffering in the observer are very great as the strength of their love makes the loss harder to bear. Indeed, it seems that suffering and love are intricately intertwined: perhaps `suffering' in all domains outside the purely physical is in some way part of the human condition associated with feeling love.
It is worth considering what happens when euthanasia is legalised and how this alters medical care. It is legal and therefore deemed by society to be a potential good - so, when it is legal it becomes a therapeutic option. And as an option there is an ethical obligation on the clinician to consider offering it to every patient who is `eligible'. We would not withhold antibiotics for an infection if the drug is available and the patient is suffering from an infection for which that treatment may be of use. The clinician looking after a patient with intractable symptoms may then offer euthanasia in ignorance of alternative strategies for relieving the distress, rather than that the distress is truly resistant to all possible interventions.
In Australia in 1998 the Northern Territories introduced the ‘Right of the Terminally Ill’ Act, later to be replaced by the Federal Parliament in Canberra. During the time the Act was in existence, seven patients were considered eligible for a life ending intervention, and four of these had their lives ended by Dr. Nitschke under the legislation. One of the patients whose life was ended believed she was dying of terminal cancer, but after death was found to have been effectively treated. Dr. Nitschke's comment to the press, the Sun Herald newspaper, four years later is interesting: he considered that it was irrelevant whether she had cancer because ‘the quality of her life was such that she thought death was preferable.’ This describes a new form of honesty developing in society, where the patient's wish to die becomes the pre-determinant of their eligibility to be killed as their continued living is causing too great a degree of suffering for them. It would appear illogical to therefore restrict euthanasia to the terminally ill who are going to die imminently anyway and to deny it to those who have made a rational suicide decision for whatever reason. At present in our society there are those who desire death and attempt to take their own life but are not suffering from a terminal illness: they are subjected to psychiatric treatment, sometimes under compulsion.
In Oregon the law allows physician-assisted suicide. Patients should have a prognosis of less than six months, although in fact only three out of four of those considered for physician assisted suicide fulfill this criterion. About one in six of those requesting physician-assisted suicide receive a prescription for a lethal overdose and one tenth take the drugs. It is worth noting that significantly more of those who receive palliative care interventions change their minds than those who do not receive such care.
Overall the evidence is that requests for physician-assisted suicide or euthanasia are often not persistently sustained over time. Patients who request euthanasia are more likely than others to feel they have been poorly investigated, have poor symptom control, and/or lack of confidence in their doctors' ability and knowledge.
Evidence from the Dutch experience shows that there are complications associated with the process of ending life. Physician-assisted suicide is usually by massive barbiturate overdose, but some patients are unable to swallow the medication or vomit it back; there are also descriptions in the scientific literature of the drugs failing to induce coma and of patients awaking again after coma. When euthanasia is resorted to, there can be difficulties accessing a vein.
There is also an impact on professionals involved in euthanasia. About three out of four of those involved in euthanasia report feelings of discomfort, described as feeling the process was burdensome, emotional and a heavy responsibility. One in twenty report subsequent doubts or regrets after the event. When life had been ended without an explicit request, the proportion feeling doubts or regret rose to 11%.
In Holland there does seem to be an effect on society of the change. Despite the claim that legalisation would result in accurate reporting of such life ending events, it seems that still only about half of all euthanasia/physician-assisted suicides are reported. Some doctors have called for the duty to report to be removed as it is administratively burdensome on the doctor. It seems that the bias in thinking towards euthanasia and physician-assisted suicide distract from other options in care, but as doctors learn more about palliative care they feel less need to resort to these life ending measures.
Different parts of the world have looked at the law in different ways. In Belgium the recently introduced legalisation of euthanasia has introduced the concept of a palliative care filter into the process. In France the debate in public reflected confusion between euthanasia and palliative care, but a committee of the French Government is due to report shortly.
It is of note that in the UK where palliative care is probably the most developed, over 95% of palliative medicine specialists do not want a change in the law to allow euthanasia/ physician-assisted suicide.
Some have described the principle of double effect as a covert form of life ending. This is untrue; those working in palliative care are clear that the evidence supports the view that giving morphine and other powerful drugs correctly does not shorten life - in fact it may prolong life as the patient is not exhausted through poor symptom control. With the concept of double effect, a predictable but unwanted effect of a drug results in the patient's death. Chemotherapy can be seen to have a double effect at times: it is given to destroy a malignancy but in some patients the fall in white count is so great that they develop neutropaenic sepsis and die from it much earlier than they would have done if treatment had not been given. However, in the context of symptom control, drugs such as morphine are titrated up to find the minimum effective dose to achieve therapeutic benefit; by contrast, when the intention is euthanasia the drug is given in a massive and purposefully lethal overdose.
So to conclude, euthanasia is a seductively simple solution to the complex problem of suffering, illness, vulnerability and the way that society responds to those requiring care. This is a complex issue for society. It is easy to make the case for the individual, but very difficult to establish the impact on (potentially) vulnerable people in the community of a change in the law to allow a doctor to kill a patient on the patient's persistent, voluntary, competent request. Perhaps it is worth remembering that no-one is isolated in their autonomy. Society is made up of people who all interact in one way or another.
Our living and our dying have an effect on those around us.
Baroness Prof. Dora Finlay of Llandaff is Dean of the Palliative Medicine Department, Velindre Hospital Whitchurch, Cardiff.
