Catholic Medical Quarterly Volume 66(4) November 2016
Parliamentary Inquiry into Freedom of Conscience in Abortion Provision
 This inquiry, chaired by Fiona Bruce MP took evidence from many sources
in July 2016. There was a 500 words limit per question. All evidence has
been made public with the report.
This inquiry, chaired by Fiona Bruce MP took evidence from many sources
in July 2016. There was a 500 words limit per question. All evidence has
been made public with the report.
The full report is available at Parliamentary Inquiry into Freedom of Conscience in Abortion http://www.conscienceinquiry.uk/
The CMA's president (Dr Philip Howard MA LLM MA MD FRCP)made the following submission.
Introduction
I am responding as an individual, however, I am President of the
Catholic Medical Association.
Profession: Consultant Physician
Please describe your interest in the questions raised by this Inquiry.
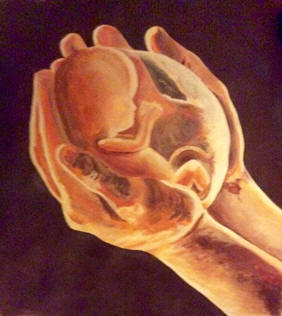
The Catholic Medical Association (CMA) The CMA was founded in 1911 as the Guild of Catholic Doctors. In 2006 the CMA became open to all practicing Catholic healthcare professionals. The CMA supports the rights of doctors and nurses to uphold the dignity of all human beings from the time of conception
INQUIRY QUESTIONS
1. Do you think freedom of conscience for healthcare professionals in the provision of abortion is important? If so, why? If not, why not?
Yes. Freedom of conscience is essential to all medical practice. Doctors and nurses are expected to act ethically and with moral integrity.
The anthropologist Margaret Mead pointed out that there was a paradigm shift with the emergence of the Medical Profession in the Hippocratic tradition when “for the first time in our tradition there was a complete separation between killing and curing”. She rightly pointed out that “The Hippocratic Oath marked one of the turning points in the history of man.” Medical practitioners were “to be dedicated completely to life under all circumstances, regardless of rank, age, or intellect; the life of the slave, the life of the Emperor, the life of a foreign land, the life of a defective child.” The absolute prohibition on direct deliberate killing is succinctly expressed in the Hippocratic Oath. “Wheresoever I go and whosoever house I enter, there will I go for the benefit of the sick, refraining from any act of wrongdoing.” (Hippocratic Oath). Medical care should be both clinically appropriate and based on sound ethical principles the most fundamental of which is respect for human life and dignity.
Freedom of conscience is fundamental to all medical practice. Clinicians must exercise not only their clinical judgement with respect to the actual needs of their patients but must act in “good faith” by exercising sound ethical judgement. Respect for life includes, at times, the duty to refrain from directly and deliberately taking life. Again, this is expressed in the Hippocratic Oath which opposes euthanasia, assisted suicide and abortion. “I will give no deadly drug to any, though it be asked of me, nor will I counsel such I will not give a woman a pessary to induce an abortion.”
Patients implicitly expect that doctors will act with integrity in their interests according to an ethical framework and respect their rights as human beings, including their right to life.
It is only comparatively recently that direct deliberate killing in the form of abortion, euthanasia and assisted suicide has been protected by legislation in Europe, North America and Canada. Freedom of conscience and the duty to respect all human life is the foundation of medical practice. Conscientious objection becomes a contingent necessity to protect ethically sound practice against direct, deliberate killing.
It is a matter of serious concern to the CMA and its members that midwives and others may be excluded from practice because of the ‘normalisation' of abortion practices and contractual requirements to be involved in procedures to which they have fundamental professional and ethical objections. This will inevitably affect the moral framework and ethos of obstetrics and those who will be recruited. It will also have an effect on those mothers who would be concerned to know that their midwives are regularly involved in feticide and abortion. Once rights of conscientious objection are denied, doctors and nurses will be under pressure to comply with the direct deliberate killing of human beings.
2. Do you think that doctors with a conscientious objection to abortion have adequate protection to fully engage in their profession without compromising their freedom of conscience?
No. There is inadequate protection for doctors with conscientious objection to abortion. The Council of Europe's Parliamentary Assembly adopted resolution 1763 in 2010 which affirms the right of conscientious objection in a medical context. In particular it provides that “no person, hospital or institution shall be coerced, held liable or discriminated against in any manner because of a refusal to perform, accommodate, assist or submit to an abortion, the performance of a human miscarriage, or euthanasia or any act that would cause the death of a human foetus or embryo, or any person.”
The GMC Guidance (2013) states in “Personal beliefs and medical practice” at paragraph 52 that “you must explain to patients if you have a conscientious objection to a particular procedure. You must tell them of their right to see another doctor and make sure they have enough information to exercise that right. In providing this information you must not imply or express disapproval of the patient’s lifestyle, choices or beliefs.”
The procurement of abortion is a criminal act unless certified by two registered medical practitioners acting “in good faith” that the exemptions under section 1 of the Abortion Act 1967 as amended by the Human Fertilisation and Embryology Act 1990, apply. Hence, prior to any referral and certification, the abortion would be unlawful except in the case of an emergency where the abortion was performed to prevent “grave permanent injury to the physical or mental health of the woman” or “risk to the life of the pregnant woman, greater than if the pregnancy were terminated.”
If doctors must act honestly and with integrity, they cannot be required to refer to others to provide the treatment to which they object on ethical grounds. This means that they cannot be expected to recommend or make referrals for procedures to which they have conscientious objections. Proposals for addressing some of the issues raised by conscientious objection to abortion are outlined in section 8.
3. Do you think that other healthcare professionals with a conscientious objection to abortion have adequate protection to fully engage in their profession without compromising their freedom of conscience?
 The
Glasgow Midwives' case focussed on the narrow issue of the scope and
meaning of conscientious objection as defined in the Abortion Act 1967
according to “the ordinary principles of statutory construction.” Clearly
the actual or presumed requirements of midwives to be involved in abortion
as if it was the same as being engaged in “all the usual care of a patient
in labour and giving birth” including “making the arrangements for the
baby once delivered” only serves to blur the distinction between the
normal practice of midwifery and deliberate abortion and feticides.
The
Glasgow Midwives' case focussed on the narrow issue of the scope and
meaning of conscientious objection as defined in the Abortion Act 1967
according to “the ordinary principles of statutory construction.” Clearly
the actual or presumed requirements of midwives to be involved in abortion
as if it was the same as being engaged in “all the usual care of a patient
in labour and giving birth” including “making the arrangements for the
baby once delivered” only serves to blur the distinction between the
normal practice of midwifery and deliberate abortion and feticides.
Crucially, freedom of conscience in relation to contractual requirements to be involved in abortion was not specifically addressed in the Glasgow Midwives' case as an Article 9 issue. Lady Hale focussed on the meaning of treatment within the Abortion Act which would be covered by the conscience clause, she did not specifically address the Article 9 issues in relation to the right to freedom of conscience, thought and belief. “Refusing for religious reasons to perform some of the duties of a job is likely (following the decision of the European Court of Human Rights in Eweida v United Kingdom ((2013) 57 EHRR 8) to be held to be a manifestation of a religious belief. There would remain difficult questions of whether the restrictions placed by the employers upon the exercise of that right were a proportionate means of pursuing a legitimate aim. The answers would be context specific and would not necessarily point to either a wide or a narrow reading of section 4 of the 1967 Act.”
A particular issue for conscientious objectors is the issue of referral. Lady Hale stated in an obiter dictum at paragraph 40 of her judgment that “it is a feature of conscience clauses generally within the health care profession that the conscientious objector be under an obligation to refer the case to a professional who does not share that objection”. Lady Hale illustrates very well the ‘normalisation' of late term abortions on the Labour Ward. She refers to two practices which pose particular problems in relation to feticide.
The first is where feticide is performed as a means of pregnancy reduction when one or more foetus is deliberately killed in utero and the pregnancy is then allowed to go to term. The second is where a late term medical abortion is undertaken but feticide is performed beforehand on the basis that there is a high expectation that the child would be born alive.
What is the moral difference between feticide immediately before delivery and infanticide afterwards? Clearly the intention in this instance is to kill the viable unborn child who would otherwise be born alive. Would a doctor or midwife be obliged to participate in, or witness, feticide in either of these cases?
The ‘normalisation' of abortion and feticide will inevitably affect the ability of conscientious midwives to engage in what they perceive to be their professional duties towards mothers and their children. If healthcare workers must act honestly and with integrity they must not be required to refer to others, or to provide the treatment to which they have conscientious objections.
4. Do you have personal experience of, or do you know of, examples of good practice where healthcare professionals do not wish to participate, directly or indirectly, in the provision of abortions? Good practice might have been shown by the healthcare professional, healthcare organisation, or both.
 Many members
of the CMA are aware of situations in which medical students, doctors or
nurses have been put at a disadvantage because of their conscientious
objections to abortions. Following one such instance of discrimination
where a trainee doctor was asked to leave his training post, the following
motion of a CMA member was passed at the BMA Annual Conference in 2009.
“That this meeting calls for all deaneries to implement appropriate
policies for equality and diversity within their training schemes
including: (1) the responsibilities of employers to have protocols to deal
with issues of conscientious objection without any individual being
disadvantaged; (ii) the responsibilities of trainees to inform the
employer of any conscientious objection issues in advance of taking up a
post.”
Many members
of the CMA are aware of situations in which medical students, doctors or
nurses have been put at a disadvantage because of their conscientious
objections to abortions. Following one such instance of discrimination
where a trainee doctor was asked to leave his training post, the following
motion of a CMA member was passed at the BMA Annual Conference in 2009.
“That this meeting calls for all deaneries to implement appropriate
policies for equality and diversity within their training schemes
including: (1) the responsibilities of employers to have protocols to deal
with issues of conscientious objection without any individual being
disadvantaged; (ii) the responsibilities of trainees to inform the
employer of any conscientious objection issues in advance of taking up a
post.”
It is rarely possible for specific instances to come to light because of the particular circumstances and issues of confidentiality. However the increasing ‘normalisation' of abortion and feticide serve to isolate those with conscientious objections to the extent that they must make conscious and individual decisions as to whether to enter certain fields of medicine and nursing. The paucity of obstetricians who do not perform any abortions is testimony to the reluctance of conscientious objectors to enter this field.
In May 2016, Professor Cathy Warwick, Chief Executive of the Royal College of Midwives and BPAS Chair backed the BPAS campaign to decriminalise abortion up to birth. She denied that there was any conflict of interest between her role in the Royal College and being Chair of BPAS and stated that “globally abortion is part of the role of the mid wife.... it is not our job really to say anything about the rights and wrongs of abortion.” In an interview with the Telegraph she stated that the medical profession are interpreting current legislation “almost as loosely as possible” to get around restrictions and that termination should be part of the “family planning jigsaw.” Midwives have strongly objected to the BPAS campaign and over 750 have signed a ‘not in our name' petition against unilateral attempts to change RCM policy by Cathy Warwick when they had not been consulted.
5. Do you have personal experience of, or do you know of, examples of poor practice where healthcare professionals do not wish to participate, directly or indirectly, in the provision of abortions? Poor practice might have been shown by the healthcare professional, healthcare organisation, or both.
 Members of the CMA are aware of situations where those with
conscientious objections to abortion and referrals have been compromised
or where their jobs or training positions are at risk. These are sensitive
and confidential at an individual level. In the Glasgow Midwives case the
nurses were clearly threatened with job losses. Such losses are likely to
occur at a local level and with rare exceptions will not come to the
attention of the public.
Members of the CMA are aware of situations where those with
conscientious objections to abortion and referrals have been compromised
or where their jobs or training positions are at risk. These are sensitive
and confidential at an individual level. In the Glasgow Midwives case the
nurses were clearly threatened with job losses. Such losses are likely to
occur at a local level and with rare exceptions will not come to the
attention of the public.
In the case of Glasgow Midwives there was an appeal as far as the Supreme Court by Greater Glasgow Health Board despite a favourable decision by the Inner House. It is clearly very difficult for individual nurses or doctors to sustain their conscientious objection to abortion and subject themselves to the stress, time and considerable costs of sustained court action over several years.
Most discrimination will occur at a local level and will not be publicised. Indeed, conscientious objectors who bring the issues to light may face the prospect of disciplinary action and job losses as seen in the case of the Glasgow Midwives.
Nevertheless, the normalisation of abortion in obstetrics and gynaecology and widespread acceptance in general practice will make it difficult for doctors and nurses to be involved in those areas of practice where the views of the healthcare professionals may be compromised. This includes GPs and trainees as well as midwives who may be pressurised to be involved in abortion and feticide on the labour ward.
6. In your view, are there any useful precedents for protection of freedom of conscience from other areas of the UK or from other jurisdictions?
There are some useful precedents for protection of freedom of conscience in relation to assisted suicide and euthanasia legislation. On the basis of such legislation, suggestions are made with respect to the law in relation to conscientious objection in Section 7.
7. Do you think legislation or professional guidance for healthcare professionals in the UK should be changed or developed? If so, in what way would you recommend?
It is important that both individuals and institutions are protected by conscience clauses in the case of abortion and feticide.
The following are suggested to conscience clauses in legislation:
- No person, or organisation, shall be under any duty (whether by any contract or arising from any statutory or other legal requirement) to participate in any act of abortion or feticide to which he has a conscientious objection.
- No hospital, nursing home, clinic or other healthcare establishment shall be under any obligation to permit or procure abortion or feticide on its premises.
- No person shall be under any duty to refer a pregnant woman for abortion or feticide to another healthcare professional.
- Any person who has a conscientious objection to engage in activities related to the procurement of abortion or feticide shall not be subject to any civil, criminal or other disciplinary sanction or penalty, or any other liability for refusing to participate in abortion or feticide.
- No medical or nursing practitioner nor any medical or nursing trainee shall be penalised by loss of their license to practice or loss of training opportunities or accreditation by virtue of their conscientious objection to abortion or feticide.
- It shall be sufficient to establish a right of conscientious objection for the person to declare such in a signed and witnessed written statement.
- Any coercion, harassment or bullying by individuals, establishments, organizations or professional bodies of those with conscientious objections to abortion or feticide shall be unlawful.
Note
For the avoidance of doubt “participation” in relation to conscientious objection to abortion and feticide includes, referrals, certification of the exceptions by two registered medical practitioners, administrative tasks preparatory to the procedures, as well as the actual performance of the abortion or feticide. In any action, the Court may take into account the context and circumstances in which the abortion or feticide occurred.
Professional bodies must not refuse accreditation or refuse a license to practice on the basis that the medical or nurse practitioner has a conscientious objection to abortion or feticide.
8. Any other comments
 The CMA is opposed to
deliberate direct abortion and feticide. Feticide is an increasing problem
in relation to late abortions where the child might otherwise be delivered
alive and in cases of selective reduction of pregnancy. It is likely to
pose problems with the advance of intrauterine interventions, therapy and
even surgery before delivery. It is important to ensure that the rights of
conscientious objection for doctors, nurses and those in training are protected. Freedom of
conscience and their right to act with honesty and integrity is essential
to the practice of medicine. Direct deliberate killing is incompatible
with the fundamental duty to respect all human life and to uphold the
dignity of all human beings. Care must be predicated on respect for human
dignity.
The CMA is opposed to
deliberate direct abortion and feticide. Feticide is an increasing problem
in relation to late abortions where the child might otherwise be delivered
alive and in cases of selective reduction of pregnancy. It is likely to
pose problems with the advance of intrauterine interventions, therapy and
even surgery before delivery. It is important to ensure that the rights of
conscientious objection for doctors, nurses and those in training are protected. Freedom of
conscience and their right to act with honesty and integrity is essential
to the practice of medicine. Direct deliberate killing is incompatible
with the fundamental duty to respect all human life and to uphold the
dignity of all human beings. Care must be predicated on respect for human
dignity.
The following are therefore suggestions as to the responsibilities of those who have conscientious objections to abortion and feticide but would also apply to physician assisted suicide and euthanasia.
Responsibilities of those with a conscientious objection to abortion and feticide.
Those with a conscientious objection should:
- Act with honesty and integrity and maintain the confidentiality of their patient.
- Explain that the objection is specific and will not affect care unrelated to abortion and especially any after care that the woman may seek.
- Make their objections known to their employers, colleagues and patients where possible in advance.
- Treat colleagues and patients who do not share those objections with respect and not take advantage of patients or cause them distress in expressing or explaining their ethical views.
- Refrain from acting or behaving as if they were making a moral judgment on others who do not share their views.
- Respect those who do not wish to discuss the ethical views regarding abortion and feticide.
- Ensure that conscientious refusal to participate in abortion should not be taken as a judgment on the action of others who may not regard abortion as wrong.
- Explain, when appropriate, why they cannot be involved in decisions regarding abortion or referrals to colleagues who provide abortion.
